Chair: Sally Benton
This session will provide an update on how new testing approaches for diagnosis of colorectal cancer and lower GI diseases are evolving.
10.15 - 10.45 - Qualitative (lateral flow) point of care FIT tests - do they work? - Shane O'Driscoll
There are an increasing number of qualitative lateral flow FIT methods available on the market. These are marketed for health care professionals and/ or public use. There is often overlap. NHS England and cancer charities have raised concerns about the availability of these kits and the validity of the results they generate. The aim of this talk is to provide an overview of kits available on the market and present results from an evaluation carried out to assess a number of these kits.
10.45 - 11.15 - A laboratory experience of calprotectin (and FIT) in clinical pathways - Neil Syme
Faecal testing has been part of the biochemical investigation of disease for a long time. The advent of more automated assays for analytes such as faecal calprotectin and haemoglobin in the last decade has led to huge improvements in diagnosis and management of lower gastrointestinal disease. Stool samples do not typically take the same route to the laboratory as blood. Collection of stool samples lies in the hands of the patient, followed by a period of storage and transport to the laboratory, where they are stored again and extracted prior to analysis. Modern faecal sample collection devices have significantly streamlined this process, enabling safer and more consistent testing, and improved workflow. This talk aims to give an overview of the implementation and challenges of stool testing in a general chemistry laboratory.
11.15 - 11.45 - Implementing faecal immunochemical testing (FIT) into symptomatic pathways the Nottingham experience - David Humes
We implemented FIT testing in our colorectal cancer pathway in Nottingham in 2016 and have developed our pathway following a successful initial pilot study. Since its introduction, we have strived to improve the ability of FIT and other factors to determine which patients should undergo invasive investigations. This has resulted in the development of the Nottingham 4F protocol of a FIT, digital rectal examination, and a full blood count and ferritin prior to referral. Through this we aim to deliver a tailored pathway to risk stratify patients and prioritise investigation in those at most risk of being diagnosed with colorectal cancer. Since its introduction, FIT has acted as a potential barrier to referral in those with symptoms and we have studied the effect sociodemographic factors have on return rates in the symptomatic population. This talk aims:
- To describe the implementation of a stratified FIT pathway and its evaluation.
- To describe variations in FIT return and use by sociodemographic factors and region.
×

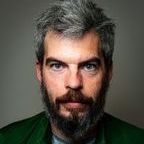
Sally Benton
Sally Benton is Consultant Clinical Scientist in Biochemistry and Clinical Lead for Clinical and Specialist Biochemistry Services at Berkshire and Surrey Pathology Services. She is also Director of the Bowel Cancer Screening South England Hub at the Royal Surrey County Hospital, Guildford. Previously Sally was Consultant Biochemist at Barts Heath NHS Trust and trained and worked at hospitals in Liverpool and Manchester between 2000 and 2008.
Sally has been working in Guildford since 2014. Her job is split between routine and specialist biochemistry services and the Bowel Cancer screening Hub. At the Bowel Cancer Hub she leads a team of research scientists who carry out research to further understand analytical aspects and clinical applications of the faecal immunochemical test for haemoglobin (FIT) and other biomarkers supporting early diagnosis of colorectal cancer. Sally and her team publish frequently in the field of FIT and early diagnosis of colorectal cancer, Sally was on the BSG/ ACP guideline group representing biochemistry. She co-chairs the World Endoscopy Organisation expert working group on FIT for Screening and is Chair of an International Federation of Clinical Chemistry working group to standardise and harmonise FIT testing.
Sally has a long standing interest in LCMS use in clinical biochemistry and this continues in BSPS with a recently established LCMS laboratory that is co-located with ICP-MS equipment and the trace elements service.
×
Shane O'Driscoll
I have been working in Bowel Cancer Screening for 12 years, and for 7 years in research. My previous work has included evaluation of FIT for Hb laboratory and POC systems, assessment of EQA materials, and NICE FIT. More recently I have been working on evaluation of faecal calprotectin methods and I am part of team for FIT in Lynch and evaluation the POC qualitative FIT devices.
×
Neil Syme
Dr Neil Syme is a Consultant Clinical Scientist in Biochemistry in NHS Lanarkshire, Scotland. He provides clinical leadership for faecal testing in Lanarkshire, and is a member of the LabMed Scientific Affairs and Clinical Practice Committee. Neil trained at the Royal Infirmary of Edinburgh, with a focus on applying mass spectrometry to endocrine and metabolic services, after which he became Deputy Director of the UK NEQAS for Peptide Hormones. In 2014, Neil moved back to clinical service provision at Glasgow Royal Infirmary, where he worked across the general and specialist endocrine sections, and managed the urine steroid profiling service. Neil has worked in Lanarkshire since 2020, and his interests include laboratory quality indicators, intelligent testing, and optimising patient testing pathways.
×
David Humes
Associate Professor of Surgical Epidemiology/Deputy Divisional Director of Surgery/Robotic Colorectal Surgeon
Mr Humes heads a research group focusing on the use of routinely collected data to study the occurrence and consequences of surgical diseases alongside delivering studies on the use of novel interventional and diagnostic devices. He has supervised 5 PhD’s to completion and his current research group includes 4 PhD students, 2 NIHR Academic Clinical Fellows and a data analyst. He has been awarded over £2.9 million in grant funding and published 108 peer-reviewed publications with a current H-index of 38 (Google Scholar). He has implemented the symptomatic FIT pathway in Nottingham. He is the current research lead for the Joint Committee on Higher Surgical Training and training lead in the NIHR BRC in Nottingham. His clinical practice focuses on robotic colorectal and anal cancer surgery.